Gastric acid secretion and peptic ulcer disease
- 1. Peptic ulcer disease Samir Haffar M.D. Assistant Professor of Gastroenterology
- 2. Functional gastric anatomy Sleisenger & Fordtran’s gastrointestinal & liver diseases. Saunders Elsevier, Philadephia, 9th ed, 2010.
- 3. Schematic representation of oxyntic gland Sleisenger & Fordtran’s gastrointestinal & liver diseases. Saunders Elsevier, Philadephia, 9th ed, 2010.
- 4. Parietal cell Electron photomicrograph Schematic representation 1 billion parietal cells line the gastric mucosa Secretes acid in response to neurocrine, paracrine & endocrine factors
- 5. Acid production by parietal cell Three secretagogues Esplugues JV. Drugs 2005 ; 65 (Suppl 1): 7 – 12. 1. Gastrin (endocrine) Produced by G cell in antrum Released into circulation 2. Acetylcholine (neurocrine) Released by vagal terminations 3. Histamine (paracrine) Stored by mast cells & ECL cells Released into interstitial fluid
- 7. Clinical features of PUD 5 – 15% of western population • Epigastric pain Burning, ill-defined aching, hunger pain 2 – 3 h after meal relieved by antacid or food Pain awakes patient from sleep (1 – 3 A.M.) • Nausea More common in GU • Weight loss More common in GU • Asymptomatic Seen in NSAID-induced ulcers • Complications Bleeding, perforation, obstruction 10% of patients present with complication
- 8. Differential diagnosis of PUD Quite extensive • Non-ulcer dyspepsia (functional dyspepsia) Up to 30% of population – Potential role of H. pylori • Gastroesophageal reflux • Proximal gastrointestinal tumors • Vascular disease • Pancreatico-biliary disease: biliary colic, chronic pancreatitis • Gastroduodenal Crohn’s disease
- 9. Alarm features in pts with suspected PUD • Age older than 55 years with new-onset dyspepsia • Family history of upper gastrointestinal cancer • Unintended weight loss • Gastrointestinal bleeding including iron deficiency • Progressive dysphagia • Persistent vomiting • Palpable mass or lymphadenopathy (Virchow's node) • Jaundice UGI endoscopy & other testing to establish the diagnosis Sleisenger & Fordtran’s gastrointestinal & liver disease. Saunders-Elsevier, Philadelphia, PA , USA, 9th edition , 2010.
- 10. Barium study of PUD Well-demarcated crater in bulb Duodenal ulcer Gastric ulcer Crater with radiating mucosal folds originating from ulcer margin Longo DL et al. Harrison’s gastroenterology & hepatology. McGraw-Hill, New York, USA, 2010.
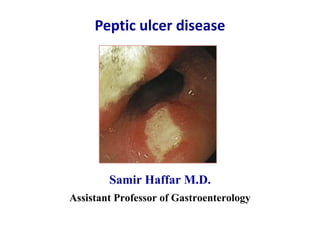
- 11. Endoscopy of PUD Mucosal break ≥ 5 mm covered with fibrin • Duodenal ulcer Bulb Kissing ulcer: 2 ulcers face to face Biopsy of antrum & body for H. pylori • Gastric ulcer Angulus of lesser curvature At any location from pylorus to cardia Biopsies to rule out malignancy • Distal duodenum Crohn’s disease, ischemia, ZES Most sensitive & specific approach
- 12. Endoscopic view of duodenal ulcer Patient with positive rapid urease test for H. pylori No history of NSAID use Sleisenger & Fordtran’s gastrointestinal & liver disease. Saunders-Elsevier, Philadelphia, PA , USA, 9th edition , 2010.
- 13. Atypical PUD • Giant ulcer Gastric ulcers > 3 cm Duodenal ulcers > 2 cm Barium studies can miss these ulcers Higher incidence of complications Higher incidence of surgery & mortality • Refractory ulcer Fail to heal despite 8-12 wks of therapy Surveillance endoscopy until healing NSAID, hypergastrinemia, ischemia ASGE guidelines. Gastrointest Endosc 2010 ; 71 : 663 – 668.
- 14. Carl Schwartz dictum: 1910
- 15. Strategies used during the 20th century for counteracting action of gastric acid Inflexion occurs during the 1980s with introduction of drugs inhibiting gastric acid secretion Dı az-Rubio M. Drugs 2005 ; 65 (Suppl. 1) : 1 – 6.
- 16. Drugs with proven effect on healing of PU • Antacids • H2-Receptor Antagonists (H2RA) • Proton Pump Inhibitors (PPI) • Mucosal protective agents Misoprostol Sucralfate Bismuth salts Malfertheiner P et al. Lancet 2009; 374 : 1449 – 61.
- 17. Antacids • Composition Aluminum & magnesium hydroxide • Mechanism Binding bile & inhibiting pepsin Promote angiogenesis in injured mucosa • Doses At least seven 30-mL doses daily • Adverse effects Diarrhea (Mg-containing agents) Constipation (Al-containing agents) Sodium overload Acid stimulation (Ca-containing agents)
- 18. H2R A (twice daily before meals) Generic name Trade Name Dose/day Cimetidine Tagamet® 800 mg Ranitidine Zantac® 300 mg Famotidine Pepcid® 40 mg Nizatidine Axid® 300 mg Competitive inhibitors of histamine stimulated acid secretion
- 19. PPIs (½ hour before meal) Generic name Trade name Standard dose Refractory patient Delayed release PPIs Omeprazole Losec® 20 mg/d 80 mg/d Lanzoprazole Lanzor® 30 mg/d 120 mg/d Pantoprazole Protonix® 40mg/d 160 mg/d Rabeprazole Pariet® 20 mg/d 80 mg/d Esomeprazole Nexium® 40 mg/d 80 mg/d Immediate release PPIs OMP bicarbonate Zegerid® 20 mg/d Block the H+K+ ATPase of parietal cell
- 20. Major metabolic pathways for various PPIs De Argila CM. Drugs 2005; 65 (Suppl 1) : 97 – 104. Pantoprazole sulfotransferase doesn't belong to CYP450 & not saturable
- 21. Which PPIs? Efficacy Esomeprazole (40mg/d) slightly more effective Useful in refractory ulcer Useful in difficult GERD: extent of lesion – Barrett’s Interactions with other drugs Less interaction in rabeprazole & especially pantoprazole Clinical relevance probably minimal Dose adjustment in AVK, benzodiazepines, phenytoin Cost considerations
- 22. When Should the PPI be Given? 15 – 30 minutes before meal Before morning meal Reduces acid secretion more than given in the evening Does not affect nocturnal acid secretion Before mid-day meal More effective inhibition of nocturnal secretion If single daily-dose Before breakfast or mid-day meals If no response Divided doses: compliance problem Increased dose (more reasonable) Gomollo n F et al. Drugs 2005; 65 (Suppl 1) : 25 – 33.
- 23. PPI dose adjustment • Renal failure No repercussion on PPI elimination No need to adjust dosage • Liver failure Half-life increases to 4 – 8 h (nl: 1 h) Reduction of dosage • Aged patients No dosage adjustment usually Adjustment if hepatic or renal failure is added to advanced age de Argila CM. Drugs 2005; 65 (Suppl 1) : 97 – 104.
- 24. Side effects of PPI No therapy is completely without risk • Osteoporosis & fractures Conflicting results • Clostridum difficile infection OR 2.05 (95% CI: 1.4-2.8) • Pneumonia OR 1.3 (95% CI: 1.1-1.4) • Acute interstitial nephritis Very rare • Iron & vit B12 deficiencies Little evidence Madanick RD. Clevland Clin J Med 2011 ; 78 : 39 – 49.
- 25. PPI & clopidogrel co-therapy Administer PPI in patients at high risk Administer PPI in all patients with dyspepsia Prefer pantoprazole or rabeprazole Weak inhibitors of CYP2C19 Pantoprazole considered the first choice PPI Separate administration by 12 – 15 hours Half life of PPI 1 – 2 h & clopidogrel 4 – 6 h PPI before breakfast & clopidogrel after dinner Lettino M. Eur J Intern Med 2011 (in press).
- 26. H2RA or PPIs? No indications for H2RA in present day digestive disease perhaps with exception of Gomollón1 F & Calvet X . Drugs 2005; 65 (Suppl 1): 25 – 33. • Management of occasional heartburn Possibly in association with an antacid • Exceptional patient who is allergic to all PPIs
- 27. PPIs are one of the most frequently prescribed classes of drug in the world because of: High level of efficacy Low toxicity Reduced cost Lack of alternative therapies
- 28. Mucosal protective agents Small role Generic name Trade Name Dose Misoprostol Prostaglandin analogue Cytotec® 200 μg qid Sucralfate Improve mucosal repair – anti-HP ® 1 g qid Bismuth salts Improve mucosal repair – anti-HP Denol® 525 mg qid Abdominal side-effects especially at higher doses
- 29. Causes & associations of PU Common forms of PU (95%) HP-associated NSAID-associated Uncommon forms of PU (5%) Acid hypersecretion: ZES – Mastocytosis Other infections: HSV1 – CMV – H. helmannii Duodenal obstruction: bands – annular pancreas Radiation-induced lesions Drugs: Chemotherapy-Biphosophonate-MFM Idiopathic Sleisenger & Fordtran’s gastrointestinal & liver disease. Saunders-Elsevier, Philadelphia, PA , USA, 8th edition , 2005.
- 30. Warren & Marshall receiving the Nobel Prize from the King Carl XVI Gustaf of Sweden Stockholm Concert Hall, 10 December 2005
- 31. Morphology of H. pylori Micro-aerophilic Gram-negative Slow growing Spiral-shaped Flagellated
- 32. Prevalence of H. pylori infection Most common chronic bacterial infection of humans 100 80 60 40 20 0 % individuals infected 0 10 20 30 40 50 60 70 80 Age (years) Marshall 1994 Developing countries Western countries 'Carrier state' from childhood infection (before 1945) Rapid acquisition in childhood
- 33. Disease associated with H. pylori infection • Gastric diseases Duodenal & gastric ulcers Non-ulcer dyspepsia Gastric cancer Gastric MALT lymphoma • Extra-gastric diseases Unexplained iron deficiency anemia Idiopathic thrombocytopenic purpura (ITP) Vitamin B12 deficiency MALT: Mucosal Associated Lymphoid Tissue
- 34. H pylori-positive ulcer • > 50% of world’s population has chronic H. pylori infection • Only 5 – 10% of those infected develop ulcers • Factors determining infection Pattern of histological gastritis Degree of acid secretion Gastric metaplasia in bulb Ulcerogenic strains Genetic factors Malfertheiner P et al. Lancet 2009; 374 : 1449 – 61.
- 35. Conditions associated with PUD Duodenal ulcer Gastric ulcer Sleisenger & Fordtran’s gastrointestinal & liver disease. Saunders-Elsevier, Philadelphia, PA , USA, 9th edition , 2010.
- 36. Natural history of H. pylori infection Longo DL et al. Harrison’s gastroenterology & hepatology. McGraw-Hill, New York, USA, 2010.
- 37. Diagnosis of H pylori infection Tests Sensitivity Specificity Non-endoscopic methods Serology ELISA IgG 85 – 92% 79 – 83% Not for confirming eradication Urea breath test 95% 96% Fecal antigen test “monoclonal” 95% 94% Endoscopic methods Rapid urease test 1 antrum & 1 corpus 98% 99% Histology 1 antrum & 1 corpus > 95% > 95% Culture 70 – 90% 100% WGO global guideline. J Clin Gastroenterol 2011 ; 45 : 383 – 388. Malfertheiner P et al. Gut 2012; 61: 646 – 664.
- 38. Urea breath test / C13 and C14 Mégraud F. Presse Med. 2010 ; 39 : 815 – 822.
- 39. Rapid Urease Test (RUT) Available RUT kits CLO test HpFast HUT-test Pronto Dry Pyloritek Overall performance of different tests comparable
- 40. Standard triple therapy (PAC) First line therapy • PPI Standard dose bid • Amoxicillin 1 g bid • Clarithromycin 500 mg bid Malfertheiner P et al. Gut 2012; 61: 646 – 664. For 7 – 10 – 14 days No indicated if clarithromycin resistance > 15 – 20%
- 41. Treatment success for triple therapy intention-to-treat analysis (ITT) Line at 80% treatment success Demarcation between acceptable & unacceptably success rate Each bar represents a different study Graham DY & Fischbach L. Gut 2010 ; 59 : 1143 – 1153.
- 42. Sequential therapy First line therapy • First 5 days PPI (standard dose, bid) Amoxicillin (1 g bid) • Second 5 days Clarihromycin (500 mg bid) Metronidazole/Tinidazole (500 mg bid) For 10 days Gisbert JP et al. J Clin Gastroenterol 2010 ; 44 : 313 – 325. Indicated in clarithromycin or nitroimidazole resistance strains No indicated in dual clarithromycin & metronidazole resistance
- 43. Concomitant therapy First line therapy • PPI Standard dose bid • Amoxicillin 1 g bid • Clarithromycin 500 mg bid • Metronidazole/Tinidazole 500 mg bid Rimbara E & Graham DY. Nat Rev Gastroenterol Hepatol 2011 ; 8 : 79 – 88. Malfertheiner P et al. Gut 2012 ; 61: 646 – 664. For 10 – 14 days No indicated in high prevalence of Clari-R (> 20 – 30%) No indicated in dual clarithromycin & metronidazole resistance
- 44. Bismuth quadruple therapy First line therapy • PPI Standard dose bid • Bismuth subsalicylate (USA) 525 mg qid Bismuth subcitrate (elsewhere) 420 mg qid • Metronidazole/Tinidazole 500 mg tid • Tetracycline 500 mg qid P Malfertheiner et al. Gut 2007 ; 56 ; 772 – 781. For 10 – 14 days Highly effective & cost effective Underutilized in clinical practice
- 45. Mégraud F. Presse Med. 2010 ; 39 : 815 – 822. Malfertheiner P et al. Gut 2012; 61: 646 – 664. Antibiotics Stopped for 4 weeks at least PPIs Stopped for 2 weeks H2RA Stopped for 7 days Antacids Not stopped Confirmation of eradication for H pylori UBT & monoclonal stool test No role for serology
- 46. Levofloxacin-based triple therapy Second line therapy • PPI Standard dose, bid • Amoxicillin 1 g, bid • Levofloxacin 500 mg, qd For 10 – 14 days Rising rates of levofloxacin resistance Malfertheiner P et al. Management of HP infection: the Maastricht IV/Florence consensus report. Gut 2012 ; 61: 646 – 664.
- 47. Culture-guided therapy Third line therapy • PPI Standard dose, bid • Bismuth 2 tablets, qid • 1st antibiotic Selected by antimicrobial sensitivity tests • 2nd antibiotic Selected by antimicrobial sensitivity tests For 10 – 14 days Malfertheiner P et al. Gut 2012 ; 61: 646 – 664.
- 48. Treatment regimen according to areas of Clari-R Region with low Clari-R prevalence (< 20%) Region with high Clari-R prevalence (> 20%) 3rd line Based on suceptibility testing only 1st line PPI-Amoxicillin-Clarithro Bismuth quadruple Bismuth quadruple Sequential or Concomitant 2nd line Bismuth quadruple PPI-Amoxicillin-Levofoxacin PPI-Amoxicillin-Levofoxacin Malfertheiner P et al. Gut 2012; 61: 646 – 664.
- 49. H. pylori & antibiotic resistance • Cross-resistance in each family of antibiotics Resistance to clarithromycin → resistance to all macrolides Resistance to levofloxacin → resistance to all fluoroquinolones • No cross-resistance between different families of antibiotics • Important to use compound indicated to get good results Clarithromycin for macrolides Tetracycline HCl and not doxycycline Levofloxacin but not ciprofloxacin for fluoroquinolones Malfertheiner P et al. Gut 2012 ; 61: 646 – 664.
- 50. Treatment of H. pylori positive peptic ulcer • Uncomplicated DU Prolonging acid inhibition with PPI not recommended after H pylori treatment • GU & complicated DU Prolonging PPI is recommended • Bleeding ulcer HP eradication started at reintroduction of oral feeding Malfertheiner P et al. Gut 2012; 61: 646 – 664.
- 51. General recommendations for H. pylori treatment • 1st line therapy Avoid CLA if given for any indication Avoid LEV if given for any indication Use 4-drug treatment: sequential, bismuth Use higher doses of drugs Use 14 day duration • 2nd line therapy Do not reuse same drugs • 3rd line therapy Use culture-guided therapy if available Graham DY & Fischbach L. Gut 2010 ; 59 : 1143 – 1153.
- 52. Pathogenesis of NSAID-induced GI injury Three main components Best Pract Res Clin Gastroenterol 2001 ; 15 : 691 – 703.
- 53. GI side effects of NSAIDs Organ Side Effects Esophagus Esophagitis – Ulcer – Stricture Ano-rectum Inflammation – Ulcer – Stricture Stomach & duodenum Subepithelial hemorrhage – Erosion – Ulcer Small Intestine Ulcers – Strictures – NSAID enteropathy Colon No pre-existing colonic disease: Ulcerations – Stricture – Diaphragm – Colitis Pre-existing colonic disease: ↑ Complications of diverticular disease Activate IBD
- 54. Complicated ulcers 1 – 1.5% in first year Clinical ulcers 4 – 5% Endoscopic ulcers 30% Relative Severity GI symptoms 40% Relative Frequency NSAID-related gastro-duodenal side effects
- 55. NSAIDs gastropathy Arthritis Rheum 1995 ; 38 : 5 – 18. Confined to mucosa Erosion Extend into submucosa Ulceration No break in mucosa Hemorrhage Endoscopic definition more practical Erosion: small & superficial Ulceration: larger ( > 5 mm) & deeper
- 56. GI safety of non-selective NSAIDs RR of different NSAIDs could differ by 10-fold * Risk at higher doses (> 1.5 –2.4 g/d) comparable to others NSAIDs Br Med J 1996 ; 312 : 1563 – 1566. Lowest risk Ibuprofen * Diclofenac Moderate risk Indomethacin Naproxen Sulindac Aspirin Highest risk Azapropazone Tolmetin Ketoprofen Piroxicam Longer half-time
- 57. Risk of UGI bleeding with aspirin Daily aspirin dose Odds ratio (95% CI) Any 3.2 (2.3 – 4.4) 75 mg 2.3 (1.2 – 4.4) 150 mg 3.2 (1.7 – 6.5) 300 mg 3.9 (2.5 – 6.3) Weil J et al. BMJ 1995 ; 310 : 827 – 30. Risk of bleeding with aspirin is dose related 75 to 300 mg/d may cause 2-3 fold increase in risk of GIT bleeding
- 58. Major GI bleeding & type of aspirin 550 incident cases & 1202 controls, 28 MA hospitals Aspirin RR of UGI bleeding ≤ 325 mg > 325 mg/day Plain 2.6 5.8 Enteric-coated 2.7 insufficient data Buffered 3.1 7.0 Kelly JP et al. Lancet 1996 ; 348 : 1413 – 16. Same risk for plain, buffered & enteric-coated aspirin
- 59. Two isoforms of cyclo-oxygenase (COX) COX-1 Housekeeping COX-2 Inflammation Regulation Constitutive Inducible Range of expression 2 – 4 fold 10 – 80 fold Tissue Expression Most tissues notably Platelets Endothelial cells Kidneys Stomach Inflammatory sites Synoviocytes Fibroblasts Monocytes
- 60. Clinical ulcer complications with COX-2 vs NSAIDs * POB: Perforation – Obstruction – Bleeding Rostom A et al. Clin Gastroenterol Hepatol 2007 ; 5 : 818 – 828. Cochrane Collaboration Systematic Review 8 studies – 73 449 patients – POB*
- 61. Prevention strategies of GI risk due to NSAIDs • Avoid use of NSAID & substitute with acetaminophen • Use “safer” NSAID: Diclofenac, ibuprofen, coxibs • Avoid NSAID with higher toxicity: Ketorolac, piroxicam • Use lowest effective dose for shortest period of time • Avoid concomitant therapy with: Anticoagulants, corticosteroids, low-dose aspirin, APT* • Eradicate HP infection in patients with prior ulcer history * APT: Anti-Platelet Therapy Sostres C et al. Best Pract Res Clin Gastroenterology 2010 ; 24 : 121 – 132.
- 62. Current ulcer therapy • H. pylori-associated PU H. pylori eradication • NSAID-associated PU PPI for healing & prevention • Small role exists for drugs enhancing mucosal resistance Malfertheiner P et al. Lancet 2009; 374: 1449 – 61.
- 63. Complications of peptic ulcer disease • Gastrointestinal bleeding (15%) First manifestation in 20% Tarry stools or coffee-ground emesis • Perforation (6 – 7%) Sudden onset of severe, generalized abdominal pain Penetration into adjacent organ: pancreatitis – gastro-colic fist • Gastric outlet obstruction (1 – 2%) Pain worsening with meals, vomiting of undigested food Inflammation & edema: resolves with ulcer healing Mechanichal: endoscopic balloon dilation – surgery Longo DL et al. Harrison’s gastroenterology & hepatology. McGraw-Hill, New York, USA, 2010.
- 64. Bleeding peptic ulcer • Most frequent cause of UGI bleeding (50%) • Especially high on gastric lesser curvature or postero-inferior wall of duodenal bulb • Most ulcer bleeding is self-limited (80%)
- 65. Laboratory evaluation • Hematocrit May not reflect blood loss accurately • Elevated BUN Not correlated to creatinine level Breakdown of blood proteins to urea Mild reduction of GFR • Iron deficiency anemia • Low MCV • Low ferritin level
- 66. Hematocrit values before & after bleeding
- 67. Forrest’s classification for PU bleeding Stage Characteristics Rebleeding I a Jet arterial bleeding 90 % Ib Oozing 50 % IIa Visible Vessel 25 - 30 % IIb Adherent clot 10 - 20% IIc Black spot in ulcer crater 7 - 10% III Clean base ulcer 3 - 5 %
- 68. Forrest’s classification for PU bleeding III (clean base)II-b (adherent clot) II-a (visible vessel)I-b (oozing) II-c (black spot) I-a (arterial jet )
- 69. MA of PPI in UGI bleeding before endoscopy 4 RCTs – 1 512 patients • Excluding pts suspected of having variceal bleeding • Rebleeding OR 0.81; 95% CI (0.61–1.09) • Endoscopic tt at subsequent index endoscopy OR 0.93, 95% CI (0.53–1.64) • Surgery OR 0.96, 95% CI (0.68–1.35) • Mortality OR 1.12; 95% CI (0.72–1.73) Dorward S et al. Cochrane Database Syst Rev 2006;(4):CD005415.
- 70. Treatment of bleeding PU • Pharmacological PPI 80 mg IV bolus 8mg / hr / 72 hours IV infusion • Endoscopic Injection (epinephrine 1/10.000) combined 2 methods Monopolar coagulation Bipolar coagulation Heater probe Hemoclips Argon plasma coagulation • Surgical When endoscopic treatment fails
- 71. PPI & bleeding PU * Barkun A et al. Ann Intern Med 2003 ;139 : 843 – 57. ** Leontiadis GI et al. Gastroenterol Clin N Am 2009 ; 38 : 199 – 213. *** Kaviani MJ et al. Aliment Pharmacol Ther 2003 ; 17 : 211 – 6. Controversial issues** • Dose No uniform consensus • Route Omeprazole 40 mg bid PO effective*** Consensus recommendations* • Initially 80 mg bolus • Followed by Infusion of 8 mg/hr for 72 hrs • After 72 h Equivalent to omeprazole 40 mg bid if oral intake is resumed
- 72. MA of PPIs in peptic ulcer bleeding 24 RCTs – 4373 patients included Leontiadis GI et al. Cochrane Database Syst Rev 2006;(1):CD002094. MortalityRebleeding – NNT 13
- 73. Free peptic ulcer perforation Chest-ray of thorax Severe generalized abdominal pain & signs of peritonitis CT usually establishes the diagnosis High mortality particularly in older adults
- 74. Contrast material in extraluminal location (lateral to duodenum) High-density ascites around liver & spleen Free peptic ulcer perforation Non-enhanced CT Johnson CD & Schmit GD. Mayo clinic gastrointestinal imaging review. Mayo Clinic Scientific Press, Rochester, MN, USA, 2005.
- 75. Peptic ulcer penetration / Posterior DU Large gastrocolic fistula due to benign gastric ulcer Johnson CD & Schmit GD. Mayo clinic gastrointestinal imaging review. Mayo Clinic Scientific Press, Rochester, MN, USA, 2005.
- 76. Peptic ulcer obstruction • Pain worsening with meals, vomiting of undigested food • Conservative management for 7–10 days Nasogastric suction, IV hydration, antisecretory agents • Endoscopic balloon dilation if obstruction persists • Surgery considered if all else fails Longo DL et al. Harrison’s gastroenterology & hepatology. McGraw-Hill, New York, USA, 2010.
- 77. Surgical treatment of PUD Substantial decrease in number of operations needed • Indications Elective: refractory ulcer – rare Urgent: complication – often • Highly selective vagotomy No drainage procedure • Vagotomy & drainage Pyloroplasty Gastroduodenostomy Gastro-jejunostomy • Vagotomy with antrectomy Billroth I or II Longo DL et al. Harrison’s gastroenterology & hepatology. McGraw-Hill, New York, USA, 2010.
- 78. Billroth I & Billroth II procedures Longo DL et al. Harrison’s gastroenterology & hepatology. McGraw-Hill, New York, USA, 2010. Billroth I often preferred over Billroth II
- 79. Retained antrum after Billroth II operation Hauser SC et al. Mayo clinic gastroenterology & hepatology board review. Mayo Clinic Scientific Press, Rochester, USA, 3rd edition, 2008. Retained antral tissue with gastrin secreting cells
- 80. Suspicion of ZES • Refractory erosive esophagitis • Multiple peptic ulcers • Ulcers in distal duodenum or jejunum • Complicated ulcers • Recurrent ulcers after acid-reducing surgery • Ulcers associated with diarrhea • Family history of MEN-1
- 81. Diagnosis of ZES
- 82. Treatment of ZES • Surgery Gastrinoma enucleation Parietal cell vagotomy Total gastrectomy (abandoned) • PPI Control acid secretion in most patients Very high doses (eg, omeprazole 120mg/day) BAO < 10 mEq/h 1 hour before next dose < 5 mEq/h in prior gastric surgery Schubert ML & Peura D A. Gastroenterology 2008 ; 134 : 1842 – 1860.
- 83. Thank You
Editor's Notes
- The stomach consists of three anatomic (fundus, corpus or body, and antrum) and two functional (oxyntic and pyloric gland) areas. The hallmark of the oxyntic gland area is the parietal cell. The hallmark of the pyloric gland area is the G or gastrin cell.
- The effects of drugs of the same pharmacological group are mostly ‘class’ or ‘group’ effectsThus all statins would have similar clinical usefulness, & all ACE inhibitors would be equally useful in management of HTN.It is not scientifically valid to assume that this is always the case.For instance, it was necessary to withdraw cerivastatin from the market because of a greater frequency of rhabdomyolysis,which was detected only during postmarketing surveillance, & it has recently been suggested that the effect of ramipril on mortality inheart failure might be greater than that of other ACE inhibitors. Scientifically valid conclusions should be based on head-to-head comparative trials between the various drugs. However, as thedemonstration of differences may be quite expensive (long-term trials with large study populations), smaller studies are usually carried out, the clinical relevance of which is quite debatable. Even more to the point: all too often, equivalence studies are accepted as valid while being methodologically clearly inadequate.The concept of bioequivalence is important because these drugs are highly labile in an acid environment and are rapidly degraded ifreleased in the stomach. the effect of a given preparation depends, not only on the amount of the active molecule contained in the capsule or tablet, but at least as much on the quality and stability of the enteric coating protecting the active molecule.The potency of these bioequivalence studies is all too often debatable.
- Administration in divided doses seems to be more effective than a single daily dose. Thus one study has shown that the same daily dose of omeprazole, administered in two divided doses (2 X 20mg), achieves a slightly better control of acid secretion than is obtainedwith single-dose administration (1 X 40mg).However, therapeutic compliance will be much more difficult to achieve in the case of divided dosage, and there are no comparative clinical studies that may allow conclusions as to whether the difference in control of gastric secretion is really relevant with respect to the therapeutic effect.
- The success of these drugs, with sales totalling $13.6 billion worldwide in 2009, is not just a result of their potency and effectivenessin improving symptoms and complications of acid-peptic disease. Their safety among pharmacologic agents has been unparalleled.Clopidogrel:on November 17, 2009, the US Food and Drug Administration (FDA) issued an alert to health care professionals and thepublic about the potential interaction between clopidogrel and omeprazole. In this alert, the FDA stated that the use of omeprazoleor esomeprazole (Nexium) with clopidogrel should be avoided.To date, only one prospective randomized controlled trial has specifically investigated the effect of PPIs on cardiovascular outcomesin patients using clopidogrel (Cogent trial). The study ended prematurely, when the sponsor suddenly and unexpectedly lost its financialBacking. Osteoporosis & fractures: Even though the studies had methodologic limitations, on May 25, 2010, the FDA announced a change in the required labeling information for PPIs to indicate a possible risk of fracture with these drugs.Acute interstitial nephritis: A systematic review from 2007 found 64 cases documented in the literature, 12 of which were considered certainly associated, and 9 of which were probably associated.
- In the past two years some scientific evidences have suggested a possible negative interference of PPIs on antiplatelet effect of clopidogrel because of the competitive inhibition of the CYP 2C19 isoenzyme.
- Barry J. Marshall receiving his Nobel Prize from His Majesty the King Carl XVI Gustaf of Sweden at the Stockholm Concert Hall, 10 December 2005.
- Serological test: serological tests are not all equivalent. Only validated IgG serology tests should be used owing to variability in the accuracy of different commercial tests.Validated IgG serology may be used in setting of recent use of antimicrobial* and antisecretory drugs, or ulcer bleeding, atrophy and gastric malignancies.Fecal antigen test:Not often used despite its high sensitivity and specificity before and after treatment.Should have a more prominent place, as it is inexpensive and noninvasive.PCR: Sensitive and specific – Not standardized.Finger-stick serology testVery poor and cannot be equated with ELISA serology
- On considère que la masse bactérienne revient à sa valeur initiale en un mois.Au cas où le malade ne pourrait arrêter son traitement antisécrétoire, la prise de pansements gastriques qui n’ont pas ces conséquences peut être envisagée.
- Rapid urease tests. Another indirect test for Helicobacter pylori, the rapid urease test, is based on metabolism of urea by urease. In this test, a mucosal biopsy is inoculated into a well that contains urea and a pH-sensitive dye (phenol red). If urease is present in the biopsy, urea in the medium is converted to NH4+, which will raise the pH. In response to an elevation in pH, the pH sensitive dye causes the well to change colors. This figure is an example of a rapid urease test, the CLOtestTM (Delta West Limited, Bentley, Western Australia). In this test, presence of H. pylori in a mucosal biopsy will be evidenced by a color change from yellow to red.
- High-dose PPIs increase cure rates by around 6 – 10% in comparison with standard doses.Increasing dose of PPI from, for example, 20 mg omeprazole twice daily to 40 mg of esomeprazole or rabeprazole twice daily may increase cure rates by 8 – 12%.Extending duration of triple therapy from 7 to 10 – 14 days improves eradication success by approximately 5% and may be considered.Penicillin allergyIn patients with penicillin allergy, in areas of low clarithromycin resistance, for a first-line treatment, a PPI-clarithromycin-metronidazole combination may be prescribed and in areas of high clarithromycin resistance, the bismuth containing quadruple therapy should be preferred.As a rescue regimen, in areas of low fluoroquinolone resistance, a levofloxacin containing regimen (together with a PPI and clarithromycin) represents a second-line alternative in the presence of penicillin allergy.
- treatment success fails to reach even 80% in most studies in the southern and central European countries of France, Italy, Spain and Turkey, populations which, as the Maastricht III report noted, tend to have a high prevalence (~18.5%) of clarithromycin resistance.triple therapy with a PPi, amoxicillin and clarithromycin should be avoided.
- We have observed that using a combination of both metronidazole and clarithromycinin quadruple regimens is very effective at eradicating strains of H pylori resistant to either clarithromycin or metronidazole. In fact, only a negligible reduction in efficacy was observed when concomitant quadruple regimens containing a PPI, amoxicillin, clarithromycin and metronidazole (a nitroimidazole), were given to patients with either nitromidazole- or clarithromycin-resistant H pylori.
- Widespread acceptance of this regimen was not forthcoming, possibly related to the requirement for dosing three or preferably four times daily, the administration of a large number of pills, a lack of availability of bismuth in many areas, and perhaps most importantly, untilrecently, the absence of a pharmaceutical sponsor to assist in education and marketing of the regimen.Capsule containing bismuth subcitrate (140 mg), metronidazole (125 mg), and tetracycline (125 mg) is available and FDA approved. The dosing is three capsules four times daily plus a PPI twice daily.
- On considère que la masse bactérienne revient à sa valeur initiale en un mois.Au cas où le malade ne pourrait arrêter son traitement antisécrétoire, la prise de pansements gastriques qui n’ont pas ces conséquences peut être envisagée.
- Antibiotic combination should be chosen according to local H pylori antibiotic resistance patterns.
- Cox-1 Inhibition:Decreased mucosal PGs synthesisDecreased of mucosal blood flow (+++).Cox-2 Inhibition:Increased neutrophils adherent to vascular epithelium Important factor of ulcer developmentTopical Irritation:Acidic NSAIDs exerts topical irritant effects leading to epithelial injury.Suppression of COX-1 causes a profound reduction of mucosal prostaglandin synthesis which probably impairs many components of mucosal defence. Among these, the reduction of mucosal blood flow may be most important. Suppression of COX-2 leads to an increase in the number of neutrophils adhering to the vascular endothelium in the gastrointestinal microcirculation, which has been shown to be an important factor in ulcer development. Many NSAIDs, particularly acidic ones, also exert topical irritant effects on the mucosa, leading to epithelial injury.
- Aspirin tablet coated with a combination of cellulose, silicon, or other inactive ingredients has resistance to disintegration in the stomach; this property allows dissolution of the drug in the more neutral to alkaline environment of the duodenum.safety of this type of product has been confirmed by several endoscopic studies that compared enteric-coated with plain aspirinpreparations in healthy volunteers with less gastric erosion and microbleeding in those who used the enteric-coated preparation.Buffering agents (calcium carbonate, magnesium oxide, and magnesium carbonate) lower hydrogen ion concentration in themicroenvironment of aspirin particles; this results in increased gastrointestinal solubility of aspirin, and reduced contact time between aspirin particles and the gastric mucosa. The expectation that buffering would reduce gastric damage has been largely unsupported by endoscopic studies. Although buffered preparations are better tolerated by some patients.Use of low doses of enteric-coated or buffered aspirin carries a three-fold increase in the risk of major UGIB. The assumption that these formulations are less harmful than plain aspirin may be mistaken.
- Pre-endoscopic administration of PPIs in patients with nonvariceal upper GI bleeding is still of controversial efficacy.The optimal dose and route of PPI administration has yet to be determined.
- RebleedingThe reduction of 30-day rebleeding rates remained statistically significant in all predetermined subgroup analyses. That is, PPIs significantly reduced rebleeding independent of methodological quality of the trials, severity of baseline endoscopic signs of recent hemorrhage, type of control treatment (placebo or H2RA), geographic location of the trials (conducted in Asia or elsewhere), mode of PPI administration (oral or intravenous), dose of PPI (high-dose defined as at least 80 mg bolus followed by an intravenous infusion of 8 mg/h for 72 hours; low-dose defined as any lesser dose intravenous or oral), and whether or not endoscopic hemostatic treatment was given.Other outcomes:Surgical interventions were significantly less common with PPI treatment (6.1%) than with control treatment (9.3%); OR 0.61, 95% CI 0.48–0.78; NNT 34, 95% CI 20–50. Further endoscopic hemostatic treatment (after randomization) was also reduced with PPIs (5.6%) compared with control treatment (15.7%); OR 0.32, 95% CI0.20–0.51; NNT 10, 95% CI 8–17.MortalityDespite the beneficial effect of PPI treatment on the above outcomes, there was no evidence of an effect on all-cause mortality rates (OR 1.01, 95% CI 0.74–1.40). PPIs significantly reduced mortality among trials that had been conducted in Asia (OR 0.35, 95% CI 0.16–0.74; NNT 34, 95% CI 20–100), but had no verifiable effect among trials that had been conducted elsewhere (OR 1.36, 95% CI 0.94–1.96). Similarly to the outcome of rebleeding, a higher treatment effect of PPIs in Asian trials was confirmed by metaregression.There have been three other published meta-analyses of RCTs that have assessed the role of PPIs in peptic ulcer bleeding. The most consistent finding of these meta-analyses, which is also in agreement with the Cochrane meta-analysis, is that PPIs compared with H2RAs or placebo significantly reduce rebleeding rates in patients with peptic ulcer bleeding.
- Peptic ulcer can also penetrate into adjacent organs, especially with a posterior DU, which can penetrate into the pancreas, colon, liver, orbiliary tree.
- Retained antrum syndrome is a rare form of hypergastrinemia in patients who have had a Billroth II operation.If a small cuff of antrum remains in the afferent limb and is excluded from exposure to gastric acid, the gastrin-producing G cells willrelease gastrin without control by the negative feedback loop, leading to hypersecretion of acid in the remaining stump.